PROOPIOMELANOCORTIN (POMC) DEFICIENCY
What causes POMC deficiency?
The main signs and symptoms of POMC deficiency include:
- Early-onset, severe obesity by age 1
- Excessive eating caused by insatiable hunger
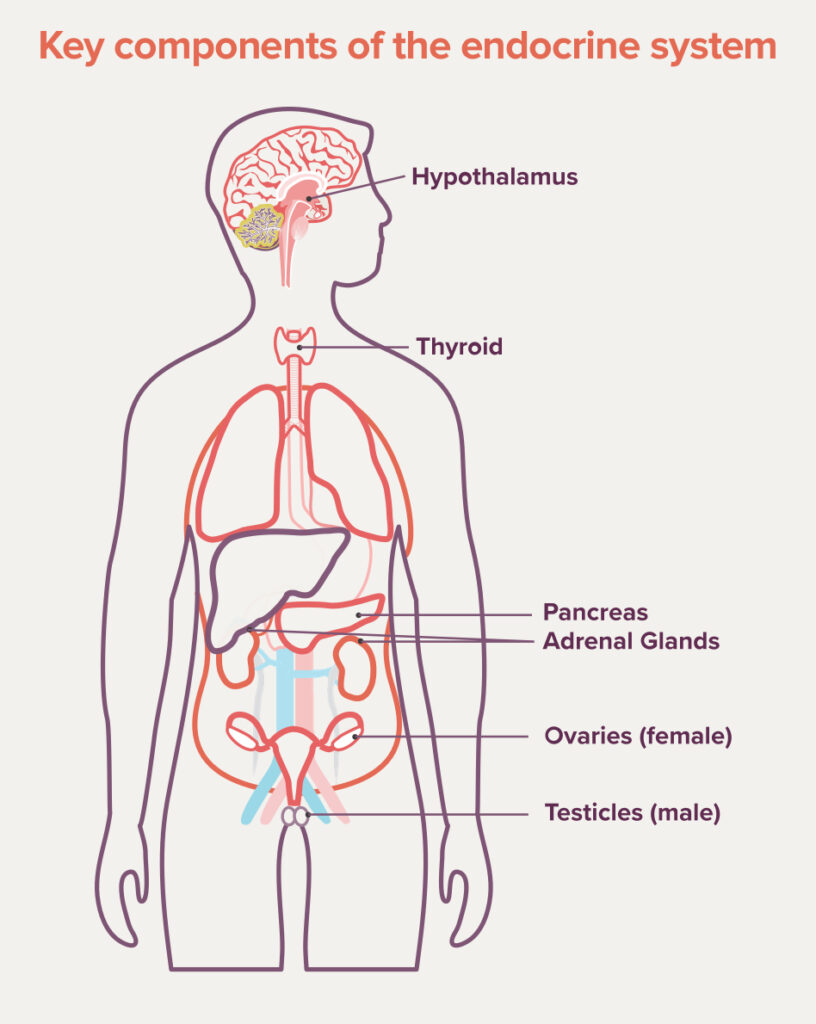
- Hormone level differences known as
endocrine abnormalities ENDOCRINE ABNORMALITIES The endocrine system is made of organs, glands, and hormones that tell the body how to do its job. This system influences how your heart beats, how you use the food you eat, how you grow, and many other important body functions. An endocrine abnormality means that one or more parts of the system is not working the way it should.
Additional signs and symptoms
Babies with POMC deficiency are typically of average birth weight and have a standard feeding schedule. But within the first few weeks of their lives, they can develop an insatiable appetite and cry constantly to be fed. Because of these symptoms, babies with POMC deficiency may start to gain weight rapidly, with their body mass index (BMI) likely falling at or above the 95th percentile for their age. Most people with POMC deficiency also continue to experience insatiable hunger and severe obesity into adult life.
Infants with POMC deficiency may also have a condition known as adrenal insufficiency, which causes low levels of adrenocorticotropic hormone (ACTH). Low levels of ACTH can lead to very low blood sugar and even seizures, and can be life-threatening without medical intervention.
Some people, but not all, may also have:
- Mildly low thyroid levels (hypothyroidismhypothyroidism
A condition caused when the thyroid doesn’t make enough of certain hormones. Symptoms of hypothyroidism include fatigue, constipation, poor temperature regulation, and thinning hair.) - Adolescent-onset growth hormone (GH) deficiencyAdolescent-onset growth hormone (GH) deficiency Growth hormone deficiency is a condition where the body does not have enough of the hormone that helps us grow. Many factors, including genetics, can cause this condition. When it begins in adolescence, it is known as adolescent-onset growth hormone deficiency.
- Delayed puberty in adolescence caused by hormonal imbalances (hypogonadotropic hypogonadismhypogonadotropic hypogonadism A rare disorder of delayed puberty that happens when levels of gonadotropin hormones (Gn) are too low, which leads to low levels of other key hormones like follicle-stimulating hormone (FSH) and luteinizing hormone (LH).)
- Red hair and light skin pigmentation
- Liver disease
POMC deficiency is inherited in an autosomal recessive autosomal recessive Autosomal recessive (AR) conditions occur when a person inherits two non-working copies of a disease-causing (pathogenic) gene variant from their parents. manner. This means that someone with POMC deficiency will have two copies of the genetic variant genetic variant Changes (also known as variants) in the standard “spelling” of a gene. Gene variants can result in serious health problems or be “silent” with no negative health effects. that causes the disorder. You can only inherit an autosomal recessive disorder if both parents are “carriers carriers In an autosomal recessive inheritance pattern, if an individual inherits one normal copy of a gene and one copy of a disease-causing variant, they are called a carrier and will generally not have any symptoms of the disease that variant causes. ” for that disorder, meaning that they both carry one copy with the genetic variant and one copy without it.
In very rare cases, someone who is a carrier for POMC deficiency (meaning they have just one disease-causing variant) may develop some of the symptoms of the disorder. This is known as POMC heterozygous deficiency.
Proprotein convertase subtilisin/kexin type 1 (PCSK1)
POMC deficiency can also be caused by a variant in the PCSK1 gene, which is also located on the MC4R pathway. People with this variant may experience symptoms like insatiable hunger, malabsorptive diarrhea, and endocrine abnormalities.
If POMC deficiency is suspected by your doctor based on clinical signs and symptoms, a genetic test can be ordered to help confirm a diagnosis.


Coping Through the Diagnostic Journey: Karen and Nate’s Story
As soon as you meet him, your face will light up. That’s who he is. Somebody once said that he was joy personified..
Nate has POMC deficiency, which is a rare genetic disorder of obesity.
KAREN
Mom to Nate, living with POMC deficiency, a rare genetic disorder of obesity
His hunger started at 1 week. He cried of hunger.
Karen: “You had dinner.”
It hurt him, and as a parent I couldn’t do anything. I couldn’t fix it.
I remember he was 5, and in 1 day, every 5 minutes, he asked for food, or referenced food, or went to the kitchen to find food. Every 5 minutes of the day.
Finding the diagnosis was a matter of me going to the doctor and saying, “There’s something wrong with my child. Look at his weight, look at his sleeping habits, look at this and this and this—I think there’s something wrong.”
The doctor walked into the room; he said, “It’s genetics, not anything you’ve done; it’s not what you fed him.”
Dealing with that information afterwards, that was difficult, because that was when I was dropped on my island. That was when I was swimming in the dark, not knowing what to do.
Social media is my lifeline. I can help people, and I can get helped in return. I talk about the bad days and the good days.
If you suspect that you or someone you know might have a rare genetic disorder of obesity, follow your instincts and talk to a doctor
I would say, go with your gut feelings. Keep going until you get the answers. You are the parent. You’re the mom, you’re the dad, whatever. You know—you know there’s something. You can feel it. You can see it. You’re with your child. Push. I’m there for them, and I hope they find answers.
Rhythm is working every day to advance the understanding of rare genetic disorders of obesity and to improve the lives of those affected
LEAD for Rare Obesity logo
www.LEADforRareObesity.com
facebook.com/LEADforRareObesity
© 2018 Rhythm Pharmaceuticals. All rights reserved. MC4R-C0089 December 2018.
See the firsthand experience of someone living with POMC deficiency

Coping Through the Diagnostic Journey: Karen and Nate’s Story
As soon as you meet him, your face will light up. That’s who he is. Somebody once said that he was joy personified..
Nate has POMC deficiency, which is a rare genetic disorder of obesity.
KAREN
Mom to Nate, living with POMC deficiency, a rare genetic disorder of obesity
His hunger started at 1 week. He cried of hunger.
Karen: “You had dinner.”
It hurt him, and as a parent I couldn’t do anything. I couldn’t fix it.
I remember he was 5, and in 1 day, every 5 minutes, he asked for food, or referenced food, or went to the kitchen to find food. Every 5 minutes of the day.
Finding the diagnosis was a matter of me going to the doctor and saying, “There’s something wrong with my child. Look at his weight, look at his sleeping habits, look at this and this and this—I think there’s something wrong.”
The doctor walked into the room; he said, “It’s genetics, not anything you’ve done; it’s not what you fed him.”
Dealing with that information afterwards, that was difficult, because that was when I was dropped on my island. That was when I was swimming in the dark, not knowing what to do.
Social media is my lifeline. I can help people, and I can get helped in return. I talk about the bad days and the good days.
If you suspect that you or someone you know might have a rare genetic disorder of obesity, follow your instincts and talk to a doctor
I would say, go with your gut feelings. Keep going until you get the answers. You are the parent. You’re the mom, you’re the dad, whatever. You know—you know there’s something. You can feel it. You can see it. You’re with your child. Push. I’m there for them, and I hope they find answers.
Rhythm is working every day to advance the understanding of rare genetic disorders of obesity and to improve the lives of those affected
LEAD for Rare Obesity logo
www.LEADforRareObesity.com
facebook.com/LEADforRareObesity
© 2018 Rhythm Pharmaceuticals. All rights reserved. MC4R-C0089 December 2018.

disease of obesity?
What treatment is available?

I think I may have a rare genetic disease of obesityWhere can I connect with people like me?